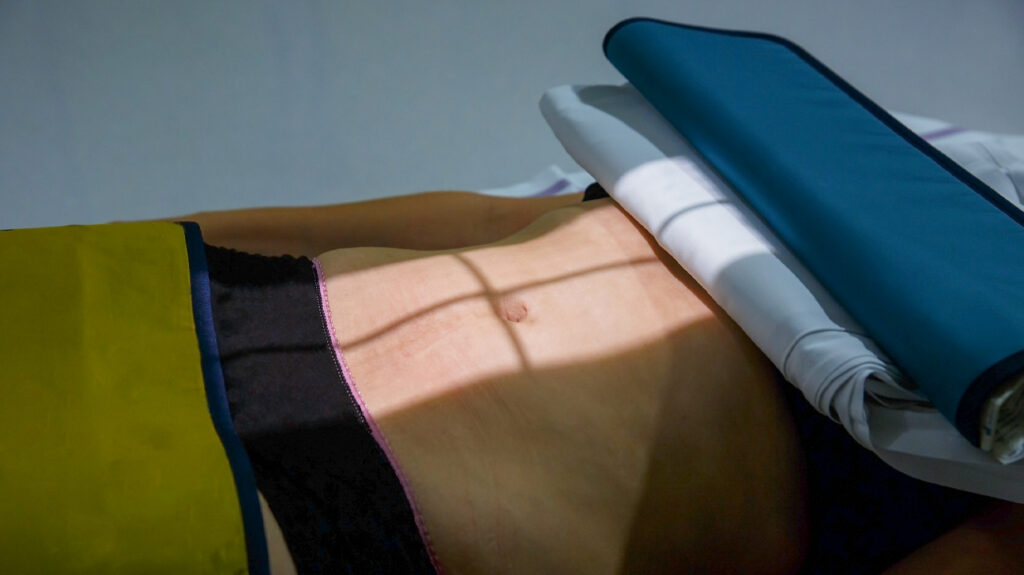
The prevalence of gastrointestinal symptoms in people with COVID-19 and what signs abdominal radiologists can look for have been illustrated by a new report.

In a new study , researchers have synthesized evidence to highlight the prevalence of gastrointestinal symptoms in people with COVID-19 from 36 scientific articles.
The research, which appears in the Abdominal Radiology journal, also identifies some of the signs that abdominal radiologists should look out for when imaging individuals.
COVID-19 unknowns
The fact that SARS-CoV-2 is a novel coronavirus has been among the challenges of the COVID-19 pandemic. SARS-CoV-2 also has several variations, though having some similarities with the previous extreme acute respiratory syndrome coronavirus (SARS-CoV) and Middle East respiratory syndrome coronavirus (MERS-CoV).
If time progresses, to find some of these unknowns, scientists may perform research on the virus and thus help guide successful policy decisions and clinical practices. This has been the case for COVID-19 symptoms.
Although scientists have been aware of the most common symptoms for some time, they have only recently recognized other less common but important symptoms: fever, coughing, loss of smell or taste, and shortness of breath.
As Dr. Mitch Wilson, a radiologist and clinical lecturer at the Faculty of Medicine & Dentistry of the University of Alberta and co-author of the report, points out, “[t]here is an increasing amount of literature demonstrating that COVID-19 is a typical presentation of abdominal symptomatology.”
The study
A team of researchers based on the increasing evidence of individuals with gastrointestinal problems associated with COVID-19 in the current report.
The researchers conducted a study to highlight patterns, challenges, or areas that need further analysis in order to do this.
Using variations of the keywords “COVID-19,” “gastrointestinal,” and “imaging,” the team searched through popular scientific databases. This resulted in 614 potentially relevant articles. A further 21 papers from other outlets were found by the team.
The researchers then deleted duplicate papers and started screening the abstracts and titles of the articles for significance, finding 137 papers.
A full-text screening was then carried out by the researchers, restricting the studies to those that involved abdominal imaging results in people who had been diagnosed with COVID-19.
The team included 36 articles in their study.
Gastrointestinal COVID-19 signs
The researchers identified two main findings after synthesizing the proof from these 36 studies.
Second, in the absence of other more well-known symptoms, gastrointestinal symptoms are a significant feature of COVID-19 and may be present.
A meta-analysis covering more than 4,200 individuals, which found 17.6 percent had gastrointestinal symptoms, was highlighted by the researchers. 16 percent emerged with only gastrointestinal symptoms in another survey of 1,141 individuals.
Second , the researchers identified a number of signs that an abdominal radiologist can look for while imaging people , especially since doctors have documented a large proportion of people with gastrointestinal symptoms with the incidental detection of COVID-19.
The symptoms that the researchers say should be searched for by abdominal radiologists include:
- Inflammation of the bowels,
- The air inside the intestinal wall,
- Perforating the intestines.
In individuals with COVID-19, however, these symptoms are relatively uncommon. Seeing these items is not actually telling us that a patient has COVID-19, as Dr. Wilson points out. It may be from a number of probable causes.
“But one of those possible triggers is virus infection, and in an area where COVID-19 is very prevalent, it is something that the referring physician must consider and possibly pose as a possibility.”