Diabetic retinopathy is the outcome of blood vessel damage in the retina caused by diabetes.
Blurred vision, difficulties seeing colors, and eye floaters are some of the symptoms of diabetic retinopathy. It can lead to eyesight loss if not treated.
Diabetic retinopathy is the most prevalent cause of vision loss in people with diabetes, as well as the primary cause of new occurrences of blindness in adults.
Although diabetic retinopathy may not have any early signs, getting a full dilated eye exam at least once a year can help a person discover the condition early and avoid consequences.
The most effective treatments to avoid diabetic retinopathy are to control diabetes and manage early symptoms.
Diabetic retinopathy is discussed in this page, along with its symptoms, symptoms, and therapies.
Diabetic retinopathy

Diabetic retinopathy is an eye condition caused by diabetes.
It can develop as a result of diabetes-related high blood sugar levels. Too much sugar in the blood can damage blood vessels throughout the body, including those in the retina, over time.
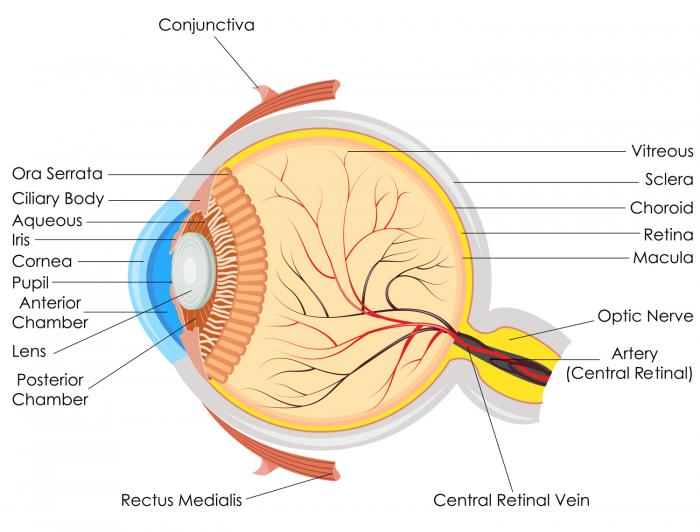
The retina is the layer of tissue that covers the back of the eye. It detects light and transmits information to the brain via the optic nerve.
Sugar can cause the retina’s small blood vessels to leak or bleed if it obstructs them. The eye may then develop new blood vessels that are weaker and more likely to leak or hemorrhage.
Proliferative diabetic retinopathy is a more advanced form of diabetic retinopathy in which the eye begins to develop new blood vessels. Nonproliferative diabetic retinopathy is the early stage.
Long durations of high blood sugar might cause the eye to fill with fluid. The fluid buildup alters the shape and curvature of the lens, producing visual abnormalities.
The lens will normally revert to its former shape and eyesight will improve if a person’s blood sugar levels are under control.
Diabetic retinopathy affects more than 2 out of every 5 people in the United States.
Other eye issues, such as cataracts and open-angle glaucoma, are also more likely to develop in people with diabetes.
Symptoms
During the early phases of diabetic retinopathy, there are generally no symptoms. When the condition is further advanced, the symptoms usually become obvious.
Both eyes are commonly affected by diabetic retinopathy. The following are some of the indications and symptoms of this condition:
- patches or streaks that block the person’s vision
- poor night vision
- a dark or empty spot in the center of the vision
- a sudden and total loss of vision
- blurred vision
- impaired color vision
- eye floaters, or transparent spots and dark strings that float in the person’s field of vision and move in the direction that the person looks
Risk factors
Diabetic retinopathy is a condition that can affect anyone who has diabetes. The risk is larger, however, if the person:
- is pregnant
- smokes regularly
- has had diabetes for a long time
- has uncontrolled blood sugar levels
- has high blood pressure
- has high cholesterol
Complications
Diabetic retinopathy can lead to a variety of consequences if left untreated.
Vitreous hemorrhage occurs when blood vessels bleed into the primary jelly that fills the eye, the vitreous. Floaters are common in moderate instances, but vision loss is more common in severe cases because the blood in the vitreous inhibits light from entering the eye.
Bleeding in the vitreous can resolve spontaneously if the retina is not injured.
Diabetic retinopathy can sometimes result in a detached retina. If scar tissue drags the retina out from the rear of the eye, this problem can occur.
It frequently causes floating dots in the person’s field of vision, as well as flashes of light and significant vision loss. If a detached retina is not treated, a person faces a substantial danger of losing their eyesight completely.
Glaucoma develops when the normal flow of fluid in the eye becomes obstructed when new blood vessels grow. The obstruction causes the risk of optic nerve injury and vision loss by causing a buildup of pressure in the eye.
Diagnosis
Diabetic retinopathy usually begins without any visible visual changes. However, an ophthalmologist, or eye expert, can discover the symptoms.
People with diabetes should get their eyes examined at least once a year or whenever their doctor suggests it.
Diabetic retinopathy can be diagnosed using the following methods:
Dilated eye exam
An eye doctor inserts drops into the patient’s eyes for a dilated eye exam. These drops dilate the pupils, allowing the doctor to see into the eye.
They’ll photograph the inside of the eye to check for the existence of:
- new blood vessels
- retinal detachment
- scar tissue
- abnormalities in the blood vessels, optic nerve, or retina
- cataracts
- changes in eye pressure
These eye drops, along with the bright lighting of the photos, might make you feel uneasy. The eye drops may induce a rise in ocular pressure in high-risk patients.
Fluorescein angiography
An eye doctor dilates the pupils with drops before injecting a dye called fluorescein into a vein in the person’s arm to conduct fluorescein angiography.
They will then photograph the dye as it flows through the eyes. If the blood arteries are aberrant, the dye may seep into the retina or discolor them.
This test can aid in determining whether blood vessels are leaking fluid, have broken down, or have been obstructed.
This information ensures that any laser treatments are carried out correctly. It can occasionally suggest that an injection of medication into the eye is required.
For a day or so after the dye has left the body, people may detect yellowish skin or dark orange urine.
Optical coherence tomography
OCT is a noninvasive imaging scan that produces high-resolution cross-sectional pictures of the retina, exposing its thickness and allowing eye specialists to check for cysts and edema.
Before and after treatments, doctors can use scans to see how effective the therapy is.
OCT is comparable to ultrasound testing, however it generates pictures with light rather than sound. The scan can also help in the diagnosis of optic nerve disorders.
Treatment
The severity of the condition and how it has reacted to past therapies all have a role in how diabetic retinopathy is treated.
In the early stages, a doctor may choose to keep a watchful eye on the patient’s eyes without interfering. The term for this strategy is “watchful waiting.”
In some circumstances, a complete dilated eye exam may be required every 2–4 months.
To control diabetes, people will need to engage with their doctors. Diabetic retinopathy can be slowed down greatly with good blood sugar management.
In most cases of severe diabetic retinopathy, surgical therapy is required.
The following options are available:
Laser treatment
Scatter laser surgery, also known as panretinal photocoagulation, is performed at an eye clinic or a doctor’s office. Targeted lasers are used by a specialist to shrink blood vessels in the eye and plug leaks caused by aberrant blood vessels.
The flow of blood and the accumulation of fluid in the eye can be stopped or slowed with this therapy. It’s possible that people will require more than one session.
The technique entails the doctor injecting numbing drugs into the eye and then using a special lens to direct a powerful beam of light into the eye.
The intense light might hurt or make you feel uneasy, and you’ll probably have impaired vision for the remainder of the day. For a few weeks following the treatment, little spots may form in the visual field.
Loss of peripheral vision, color vision, and night vision are all concerns associated with laser therapy. A person can discuss the relative advantages and dangers of this treatment with their doctor.
Injections
Certain medications can help to lessen edema and blood vessel leaking in the eyes. Anti-VEGF medicines and corticosteroids are examples of medications.
The doctor administers eye injections by performing the following procedures:
- placing numbing medicine on the eye
- cleaning the eye to help prevent infections
- placing the medicine in the eye using a very small needle
People may require regular injections at first, but they normally require less doses over time.
Eye surgery
A vitrectomy may be beneficial if a person’s retina or vitreous is causing them troubles. A portion of the vitreous from the eye is removed during this treatment.
This treatment will be performed in a hospital under general or monitored anesthesia by a surgeon.
The goal is to enhance vision by replacing clouded vitreous or blood, as well as to assist the doctor in locating and repairing any causes of retinal hemorrhage.
The surgeon will replace the hazy or bloody vitreous with a clear liquid or gas once it has been removed. Over time, the body will absorb the liquid or gas and replace it with fresh vitreous.
The person will normally need to wear an eye patch for approximately a day after the operation and use eye drops to minimize swelling and avoid infections.
If a gas bubble is inserted into the eye, the patient must maintain their head in a specific posture for a few days or weeks to ensure that the bubble remains in place. They’ll also have to avoid flying and visiting high-altitude locations until the bubble dissipates.
Diabetic retinopathy surgery is not a cure, although it can help to stop or decrease the progression of symptoms. Diabetes is a long-term condition, and even with therapy, retinal damage and visual loss can occur.
Prevention
Diabetic retinopathy can be avoided if blood sugar levels are properly managed.
Early diagnosis of symptoms improves the treatment’s efficacy.
Hypertension, or high blood pressure, is another risk to consider. People with diabetes can regulate their blood pressure by doing things like:
- moderating their alcohol intake
- taking any antihypertensive measures that the doctor recommends
- attending regular screenings
- exercising regularly
- reaching or maintaining a moderate body weight
- eating a healthful and balanced diet
- quitting smoking
Conclusion
Diabetic retinopathy is a type of eye condition that affects people. It can lead to issues, including vision loss, if not treated.
A full dilated eye exam should be done at least once a year to identify the condition early and avoid consequences.
Sources:
- https://www.aao.org/eye-health/diseases/what-is-diabetic-retinopathy
- https://www.medicalnewstoday.com/articles/183417
- https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/diabetic-retinopathy
- https://www.cdc.gov/visionhealth/pdf/factsheet.pdf
- https://beavrs.org/diabetic-vitreous-haemorrhage