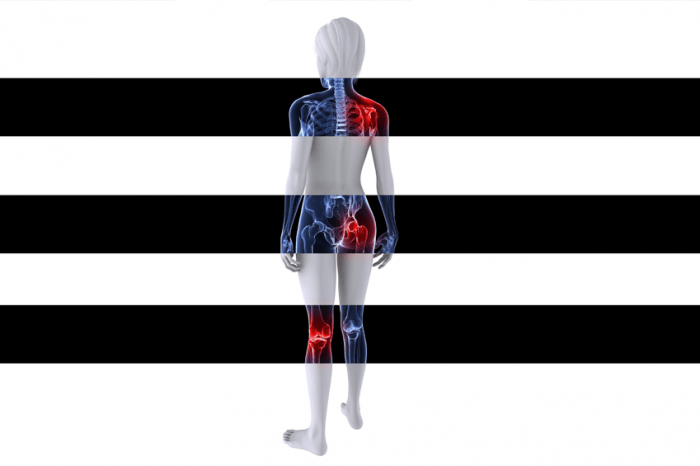
Arthritis means joint inflammation but the term is used to describe about 200 disorders affecting joints, tissues surrounding the joint, and other connective tissues. It is a state of rheumatoid arthritis.
Osteoarthritis is the most common type of Arthritis. Many severe arthritis-related rheumatoid arthritis disorders include gout, fibromyalgia and rheumatoid arthritis ( RA).
Rheumatic disorders tend to cause pressure, pain , stiffness and swelling of one or more joints and around it. The symptoms that slowly or abruptly grow. Some forms of rheumatoid arthritis may also include the body’s immune system and various internal organs.
Some forms of arthritis can affect multiple organs and cause widespread symptoms, such as rheumatoid arthritis and lupus (SLE).
54.4 million people in the United States have been diagnosed with some form of arthritis according to the Centers for Disease Control and Prevention ( CDC). For these, by their disability 23.7 million people have in some way curtailed their operation.
Arthritis is more common in adults 65 years of age or older, but can affect people of all ages, including babies.
Important facts about arthritis
- Arthritis refers to around 200 rheumatic diseases and conditions that affect joints, including lupus and rheumatoid arthritis.
- It can cause a range of symptoms and impair a person’s ability to perform everyday tasks.
- Physical activity has a positive effect on arthritis and can improve pain, function, and mental health.
- Factors in the development of arthritis include injury, abnormal metabolism, genetic makeup, infections, and immune system dysfunction.
- Treatment aims to control pain, minimize joint damage, and improve or maintain quality of life. It involves medications, physical therapies, and patient education and support.
Treatment

Arthritis treatment aims at pain management, reducing joint damage, and enhancing or preserving function and quality of life.
A range of lifestyle and medication strategies can help achieve this and protect the joints from further damage.
Possible treatment may include:
- medications
- non-pharmacologic therapies
- physical or occupational therapy
- splints or joint assistive aids
- patient education and support
- weight loss
- surgery, including joint replacement
Medication
Non-inflammatory types of arthritis, such as osteoarthritis, are often treated with pain-reducing medications, physical activity, weight loss if the person is overweight, and self-management education.
Such therapies also refer to inflammatory arthritis types, such as RA, along with anti-inflammatory medications, such as corticosteroids and non-steroidal anti-inflammatory drugs (NSAIDs), anti-rheumatic disease-modifying medications (DMARDs), and a relatively new class of drugs known as biologics.
Medicines may depend on the Arthritis type. Drugs which are widely used include:
- Analgesics: these reduce pain, but have no effect on inflammation. Examples include acetaminophen (Tylenol), tramadol (Ultram) and narcotics containing oxycodone (Percocet, Oxycontin) or hydrocodone (Vicodin, Lortab).
- Non-steroidal anti-inflammatory drugs (NSAIDs): these reduce both pain and inflammation. Some NSAIDs are available as creams, gels or patches which can be applied to specific joints.
- Counterirritants: some creams and ointments contain menthol or capsaicin, the ingredient that makes hot peppers spicy. Rubbing these on the skin over a painful joint can modulate pain signals from the joint and lessen pain.
- Disease-modifying antirheumatic drugs (DMARDs): used to treat RA, DMARDs slow or stop the immune system from attacking the joints. Examples include methotrexate (Trexall) and hydroxychloroquine (Plaquenil).
- Biologics: used with DMARDs, biologic response modifiers are genetically engineered drugs that target various protein molecules involved in the immune response. Examples include etanercept (Enbrel) and infliximab (Remicade).
- Corticosteroids: prednisone and cortisone reduce inflammation and suppress the immune system.
Natural remedies
A healthy, balanced diet with regular exercise, avoiding smoking and not consuming too much alcohol will help people with arthritis improve their overall health.
Diet
There is no particular diet that prevents arthritis, but some food types may help minimize inflammation.
Foods found in a Mediterranean diet can provide numerous nutrients that are good for common health:
- fish
- nuts and seeds
- fruits and vegetables
- beans
- olive oil
- whole grains
Foods to avoid
There are some items that arthritis sufferers may want to avoid.
Night shade vegetables, such as tomatoes, contain a chemical called solanine that has been related to arthritis pain by some studies. Research results are inconsistent when it comes to these vegetables, but some people have reported a reduction in symptoms of arthritis while removing vegetables from night shade.
Self-management
Self-management of arthritis symptoms is also important.
Key strategies include:
- staying physically active
- achieving and maintaining a healthy weight
- getting regular check-ups with the doctor
- protecting joints from unnecessary stress
Seven habits that can help a person with arthritis to manage their condition are:
- Being organized: keep track of symptoms, pain levels, medications, and possible side effects for consultations with your doctor.
- Managing pain and fatigue: a medication regimen can be combined with non-medical pain management. Learning to manage fatigue is key to living comfortably with arthritis.
- Staying active: exercise is beneficial for managing arthritis and overall health.
- Balancing activity with rest: in addition to remaining active, rest is equally important when your disease is active.
- Eating a healthful diet: a balanced diet can help you achieve a healthy weight and control inflammation. Avoid refined, processed foods and pro-inflammatory animal-derived foods and choose whole plant foods that are high in antioxidants and that have anti-inflammatory properties.
- Improving sleep: poor sleep can aggravate arthritis pain and fatigue. Take steps to improve sleep hygiene so you find it easier to fall asleep and stay asleep. Avoid caffeine and strenuous exercise in the evenings and restrict screen-time just before sleeping.
- Caring for joints: tips for protecting joints include using the stronger, larger joints as levers when opening doors, using several joints to spread the weight of an object such as using a backpack and gripping as loosely as possible by using padded handles.
Do not sit in the same position for long periods. Take regular breaks to keep mobile.
Physical therapies
Doctors will often recommend a physical therapy course to help arthritis patients overcome some of the challenges, and reduce mobility limitations.
Forms of recommendable physical therapy can include:
- Warm water therapy: exercises in a warm-water pool. The water supports weight and puts less pressure on the muscles and joints
- Physical therapy: specific exercises tailored to the condition and individual needs, sometimes combined with pain-relieving treatments such as ice or hot packs and massage
- Occupational therapy: practical advice on managing everyday tasks, choosing specialized aids and equipment, protecting the joints from further damage and managing fatigue
Physical activity
Evidence indicates that while individuals with arthritis can experience short-term pain increases when starting exercise first, continued physical activity can be an effective way to minimize long-term symptoms.
Arthritis patients may engage in joint physical activity either on their own or with friends. Given that many people with arthritis have another illness, such as heart disease, choosing suitable activities is important.
Joint physical activities appropriate for arthritis- and heart disease adults include:
- walking
- swimming
- cycling
A health care provider will help you find ways to lead a safe lifestyle and a better quality of life.
Natural therapies
A variety of alternative treatments to different forms of arthritis have been proposed.
Some work has supported the use of Devil’s claw, rosehip, and Boswellia, from the Frankincense tree, according to the organization Versus Arthritis, based in the UK.
There is some evidence that turmeric can help, but to confirm their efficacy, further studies are needed.
RA has been recommended for various other herbs and spices, but more research is needed again. Among them are turmeric, garlic , ginger, black pepper and green tea.
Anyone who is considering using natural remedies for any form of arthritis should talk to a doctor first.
Causes
Both forms of arthritis are not caused singlely. The cause or causes differ depending on the Arthritis type or form.
Possible causes may include:
- injury, leading to degenerative arthritis
- abnormal metabolism, leading to gout and pseudogout
- inheritance, such as in osteoarthritis
- infections, such as in the arthritis of Lyme disease
- immune system dysfunction, such as in RA and SLE
Most forms of arthritis are associated with a variety of causes, but some have no apparent cause and in their appearance seem unpredictable.
Some people may have a greater genetic probability of developing certain arthritic conditions. Additional factors, such as prior injury , illness, smoking and physically demanding occupations, may interfere with genes to increase the risk of arthritis even further.
Diet and nutrition can play a role in controlling arthritis and the likelihood of arthritis, while arthritis is not known to cause particular foods, food sensitivities or intolerances.
Foods that increase inflammation, especially foods derived from animals and diets high in refined sugar, can intensify the symptoms, as can eating foods that cause an immune response.
Gout is one form of arthritis closely associated with food, as it is caused by elevated levels of uric acid that can result from a diet high in purines.
Diets containing high-purine foods such as fish, red wine, and meats can cause a flare-up in gout. However, vegetables and other plant foods which contain high purine levels do not seem to exacerbate the symptoms of gout.
Risk factors for arthritis
Arthritis has been linked with some of the risk factors. Some of these can be changed while others can not.
Non-modifiable arthritis risk factors:
- Age: the risk of developing most types of arthritis increases with age.
- Sex: most types of arthritis are more common in females, and 60 percent of all people with arthritis are female. Gout is more common in males than females.
- Genetic factors: specific genes are associated with a higher risk of certain types of arthritis, such as rheumatoid arthritis (RA), systemic lupus erythematosus (SLE) and ankylosing spondylitis.
Modifiable arthritis risk factors:
- Overweight and obesity: excess weight can contribute to both the onset and progression of knee osteoarthritis.
- Joint injuries: damage to a joint can contribute to the development of osteoarthritis in that joint.
- Infection: many microbial agents can infect joints and trigger the development of various forms of arthritis.
- Occupation: certain occupations that involve repetitive knee bending and squatting are associated with osteoarthritis of the knee.
Comorbidities
In the United States, over half of adults with arthritis report high blood pressure. High blood pressure is associated with heart disease, the most prevalent comorbidity of arthritis among adults.
Around one in five U.S. adults suffering from arthritis are smokers. Smoking is associated with chronic respiratory problems, the second most prevalent comorbidity of arthritis in adults.
Types
There are about 200 types of arthritis, or conditions in the musculoskeleton. These are divided into seven main categories:
- Inflammatory arthritis
- Degenerative or mechanical arthritis
- Soft tissue musculoskeletal pain
- Back pain
- Connective tissue disease
- Infectious arthritis
- Metabolic arthritis.
Inflammatory arthritis
Inflammation is a common part of healing process in the body. The inflammation tends to occur as a defense against bacteria and viruses, or as a response to injuries such as burns. However, inflammation occurs in humans for no specific cause, with inflammatory arthritis.

Inflammatory arthritis is characterized by damaging inflammation, which does not occur as a normal injury or infection reaction. This type of inflammation is unhelpful, causing damage to the affected joints and leading to pain , stiffness and swelling.
Inflammatory arthritis can affect several joints, and the inflammation can damage both the joint surface and the underlying bone as well.
Examples include inflammatory arthritis:
- Rheumatoid arthritis (RA)
- Reactive arthritis
- Ankylosing spondylitis
- Arthritis associated with colitis or psoriasis
The word “arthritis” means “joint inflammation,” but inflammation may also affect the tendons and ligaments surrounding the joint.
Degenerative or mechanical arthritis
Degenerative or mechanical arthritis refers to a group of conditions that involve predominantly cartilage damage covering the ends of the bones.
The primary role of the smooth, flexible cartilage is to help the joints glide smoothly and move. That form of arthritis makes the cartilage thinner and rougher.
In an attempt to regain cohesion, the body begins remodeling the bone to compensate for the loss of cartilage and changes in joint function. This can trigger the production of undesirable bony growths, called osteophytes. The joint can become disfigured. That condition is commonly referred to as osteoarthritis.
Osteoarthritis can also result from previous damage to the joint such as a fracture or previous inflammation in the joint.
Soft tissue musculoskeletal pain
In tissues other than the joints and bones soft tissue musculoskeletal pain is felt. After injury or overuse, such as tennis elbow, the pain often affects a part of the body and originates from the muscles or soft tissues that support the joints.
Fibromyalgia can be characterized by pain that is more common and associated with other symptoms
Back pain
Muscles, muscles , nerves, ligaments, bones, or joints may cause back pain. Back pain may be attributed to complications within the body with organs. Of example, it may also be the product of referred pain when an problem elsewhere in the body contributes to back pain.
There could be a particular cause, including osteoarthritis. When it occurs in the spine this is often called spondylosis. That can be detected by imaging tests or physical examination.
Another source of back pain is a “slipped” joint, as is osteoporosis, or bone thinning.
If a doctor is unable to determine the exact cause of back pain, this is sometimes referred to as “non-specific” pain.
Connective tissue disease (CTD)
Connective tissue supports, binds together or separates tissues and organs from other bodies. They are composed of tendons , ligaments and cartilage.
CTD involves pain and inflammation in the joints. Many tissues, including the skin , muscles, lungs , and kidneys, can also experience inflammation. Aside from painful joints, this may result in multiple symptoms and may require consultation with a variety of different specialists.
Examples of CTD include:
- SLE, or lupus
- scleroderma, or systemic sclerosis
- dermatomyositis.
Infectious arthritis
A bacterium, virus, or fungus that enters a joint can sometimes cause inflammation.
Organisms that can infect joints include:
- Salmonella and Shigella, spread through food poisoning or contamination
- chlamydia and gonorrhea, which are sexually transmitted diseases (STDs)
- hepatitis C, a blood-to-blood infection that may be spread through shared needles or transfusions
An infection in the joint may also be cleansed with antibiotics or other antimicrobial drugs. However, the arthritis can sometimes become chronic, and if the infection has persisted for some time, joint damage may be irreversible.
Metabolic arthritis
Uric acid is a chemical that is formed by breaking down substances called purines. Purines are present in human cells, as well as in other foods.
Most uric acid is dissolved in blood and transported to the kidneys. It passes out into urine from there. Some people have high uric, acid levels because either they produce more naturally than they need or their bodies can not clear up the uric acid quickly enough.
In certain people uric acid builds up and accumulates needle-like crystals in the joint, resulting in unexpected bursts of severe joint pain or gout attack.
When uric acid levels are not decreased, gout can either come and go in episodes or become chronic.
This usually affects a single joint or a few joints, such as the broad toe and hands. The extremities are typically affected by it. One theory is uric acid crystals are formed in cooler joints, away from the body’s main warmth.
Below we describe some of the more common forms of arthritis.
Rheumatoid arthritis

Rheumatoid arthritis ( RA) occurs when the body’s immune system attacks the body’s tissues, particularly the connective tissue, leading to joint inflammation , pain and joint tissue degeneration.
Cartilage is a flexible, connective joint tissue which absorbs the pressure and shock produced by movement such as running and walking. Often it supports the joints and allows smooth movement.
Persistent inflammation within the synovia contributes to cartilage and bone degeneration. This can lead to deformity, pain , swelling and redness in the joint.
RA can appear at any age, and is associated with fatigue after rest and prolonged rigidity.
RA causes premature mortality and disability and can jeopardize living standards. Conditions it is associated with include cardiovascular diseases, such as heart disease and stroke.
Early diagnosis of RA gives a better chance of learning how to successfully manage the symptoms. This may reduce the disease’s effect on quality of life.
Osteoarthritis

Osteoarthritis is a severe degenerative joint condition affecting a joint’s cartilage, joint lining, ligaments and underlying bone.
The breakdown of these tissues eventually results in discomfort and stiffness in the joints.
The joints most commonly affected by osteoarthritis are those that undergo heavy use, such as hips , knees, hands, spine, thumb base and big toe joint.
Childhood arthritis
That may refer to a number of arthritis types. The most common form is juvenile idiopathic arthritis (JIA) which is also known as juvenile rheumatoid arthritis (JRA).
Arthritis can cause permanent damage to joints during childhood, and there is no cure. Remission, however, is possible, during which time the illness remains inactive.
This may be due to problems with the immune system.
Septic arthritis
Within the general population, this is thought to affect between 2 and 10 people in every 100,000. It can affect 30 to 70 people per 100,000, including people with RA.
Septic arthritis is an inflammation of the joints caused by a bacterial or fungal infection. It most usually affects the hip and knee.
It can grow when bacteria or other micro-organisms that cause disease spread through the blood to a joint, or when the joint is directly infected with a micro-organism through injury or surgery.
Most cases of acute septic arthritis cause bacteria such as Staphylococcus, Streptococcus, or Neisseria gonorrhoeae. Organisms including Mycobacterium tuberculosis and albicans Candida cause chronic septic arthritis. This is less severe as compared to acute septic arthritis.
Septic arthritis can develop at any age. This can occur in infants before age 3. At this age the hip is a common infection site.
Septic arthritis from 3 years before puberty is rare. Children with septic arthritis are more likely to get diagnosed with Group B Streptococcus or Haemophilus influenzae than adults because they have been vaccinated.
Incidence of H-infection causing bacterial arthritis. Influenzae decreased from use of H by around 70 percent to 80 percent. Vaccine against influenzae b (Hib) has become widespread.
Subsequent conditions raise the risk of septic arthritis:
- existing joint disease or damage
- artificial joint implants
- bacterial infection elsewhere in the body
- presence of bacteria in the blood
- chronic illness or disease (such as diabetes, RA and sickle cell disease)
- intravenous (IV) or injection drug use
- medications that suppress the immune system
- recent joint injury
- recent joint arthroscopy or other surgery
- conditions such as HIV, that weaken immunity
- diabetes
- older age
Septic arthritis is an emergency in rheumatology, because it can lead to rapid joint destruction. It may be fatal.
Fibromyalgia
Fibromyalgia affects an estimated 4 million people, or around 2 percent of the population, in the United States.
It usually begins during or after middle age, but may affect children.
Fibromyalgia can involve:
- widespread pain
- sleep disturbance
- fatigue
- depression
- problems with thinking and remembering
The person may experience an abnormal processing of pain, where they strongly react to something other people would not find painful.
Tingling or numbness can also occur in the hands and feet, jaw pain and digestive problems.
Fibromyalgia causes are unclear but certain factors have been strongly linked with the development of the disease:
- stressful or traumatic events
- post-traumatic stress disorder (PTSD)
- injuries due to repetitive movements
- illness, for example viral infections
- having lupus, RA, or chronic fatigue syndrome
- family history
- obesity
It is more common among females.
Psoriatic arthritis
Psoriatic arthritis is a joint disorder that also occurs with psoriasis, a skin disease. About 0.3 and 1 percent of the U.S. population, and between 6 and 42 percent of people with psoriasis are thought to be affected.
Most people with psoriatic arthritis and psoriasis experience first psoriasis and then psoriatic arthritis but sometimes joint problems may arise before skin lesions appear.
The exact cause of psoriatic arthritis is not clear but it seems to include an attack on healthy cells and tissue by the immune system. The abnormal immune response triggers joint inflammation, and skin cell overproduction. It can result in damage to joints.
Factors that increase the risk, include:
- having psoriasis
- family history
- being aged from 30 to 50 year
Individuals with psoriatic arthritis appear to have a higher number of cardiovascular disease risk factors compared to the population including increased BMI, triglycerides and C-reactive protein.
Gout
Gout is a rheumatic disease that occurs in body tissues and fluids when uric acid crystals, or monosodium urate, form in. It occurs when too much uric acid is released by the body, or not enough uric acid is absorbed.

Acute gout normally appears as a severely red, hot, and swollen joint and severe pain.
Risk factors include:
- overweight or obesity
- hypertension
- alcohol intake
- use of diuretics
- a diet rich in meat and seafood
- some common medicines
- poor kidney function
Long remission periods are possible, followed by flares which last from days to weeks. That can be chronic at times. Recurring acute gout attacks may lead to a degenerative form of chronic arthritis called gouty arthritis.
Sjögren’s syndrome
Sjögren ‘s syndrome is an autoimmune disease, which happens alongside RA and SLE at times. It involves destruction of the tears and saliva generating glands. This induces dryness in the mouth and eyes, and in other places that normally need moisture, such as the nose , throat, and skin.
The joints, lungs , kidneys, blood vessels, digestive organs, and nerves can also be affected.
Sjögren ‘s syndrome usually affects people aged between 40 and 50 years, and women in particular.
According to a study in Clinical and Experimental Rheumatology, the condition affects tissues other than the glands in 40 to 50 percent of people with primary Sjögren syndrome.
It may affect the lungs, liver, or kidneys, or it may lead to vasculitis in the skin, peripheral neuropathy, glomerulonephritis, and low levels of a substance called C4. These all indicate a link between the immune system and Sjögren’s.
If these tissues are impaired, the risk of developing lymphoma that is not Hodgkin’s is high.
Scleroderma
Scleroderma refers to a category of diseases affecting the body’s connective tissue. The person will have hairy, dry skin patches. Many types may affect the small arteries and internal organs.
Scar-like tissue builds up and causes damage in the skin.
The cause is not yet understood. It often affects people between 30 and 50 years of age, and can occur with other autoimmune diseases, such as lupus.
Scleroderma affects people differently. The risks include skin issues, heart failure, damage to the lungs, stomach problems and kidney failure.
Systemic lupus erythematosus (SLE)
SLE, also known as lupus, is an inflammatory disease in which the immune system develops antibodies to cells in the body that cause widespread inflammation and damage to the tissues. The disorder is characterized by periods of recovery and sickness.
It can occur at any age but most likely it will start between the ages of 15 and 45. Between 4 and 12 women will do so for every single man who gets lupus.
Lupus has the potential to affect joints, skin, brain, lungs , kidneys, blood vessels and other tissues. Symptoms include fatigue, joint pain or swelling, rashes in the skin and fevers.
The cause remains unknown but it may be associated with genetic , environmental, and hormonal factors.
Early signs
The arthritis symptoms that occur and how they occur differ greatly, depending on the condition.

They may increasingly or suddenly develop. Since arthritis is most commonly a chronic disease, symptoms can come and go, or may persist over time.
Anyone experiencing any of the following four key warning signs should see a doctor though.
- Pain: Pain from arthritis can be constant, or it may come and go. It may affect only one part, or be felt in many parts of the body
- Swelling: In some types of arthritis the skin over the affected joint becomes red and swollen and feels warm to the touch
- Stiffness. Stiffness is a typical symptom. With some types, this is most likely upon waking up in the morning, after sitting at a desk, or after sitting in a car for a long time. With other types, stiffness may occur after exercise, or it may be persistent.
- Difficulty moving a joint: If moving a joint or getting up from a chair is hard or painful, this could indicate arthritis or another joint problem.
Rheumatoid arthritis
RA is a systemic condition, and the joints on both sides of the body are typically affected similarly. The most often affected are the joints of the wrists, fingers, knees, feet and ankles.
Joint symptoms may include:
- morning stiffness, lasting more than 1 hour
- pain, often in the same joints on both sides of the body
- loss of range of motion of joints, possibly with deformity
Other symptoms include:
- chest pain when breathing in, due to pleurisy
- dry eyes and mouth, if Sjögren’s syndrome is present
- eye burning, itching, and discharge
- nodules under the skin, usually a sign of more severe disease
- numbness, tingling, or burning in the hands and feet
- sleep difficulties
Osteoarthritis
Osteoarthritis is typically the result of joint wear and tear. It will affect overworked joints more than others. Osteoarthritis sufferers can develop the following symptoms:
- pain and stiffness in the joints
- pain that becomes worse after exercise or pressure on the joint
- rubbing, grating, or crackling sound when a joint is moved
- morning stiffness
- pain that causes sleep disturbances
Some people may have osteoarthritis-related changes that occur in an x-ray but they do not feel symptoms.
Osteoarthritis is usually more likely to impact some joints than others, such as left or right knees, shoulder or wrist.
Childhood arthritis
Symptoms of childhood arthritis include:
- a joint that is swollen, red, or warm
- a joint that is stiff or limited in movement
- limping or difficulty using an arm or leg
- a sudden high fever that may come and go
- a rash on the trunk and extremities that comes and goes with the fever
- symptoms throughout the body, such as pale skin, swollen lymph glands
- generally appearing unwell
Also, juvenile RA can cause eye problems, such as uveitis, iridocyclitis or iritis. When eye symptoms are present they can include:
- red eyes
- eye pain, especially when looking at light
- vision changes.
Septic arthritis
Symptoms of septic arthritis occur rapidly.
There is often:
- fever
- intense joint pain that becomes more severe with movement
- joint swelling in one joint
Symptoms in newborns or infants include:
- crying when the infected joint is moved
- fever
- inability to move the limb with the infected joint
- irritability
Symptoms in children and adults include:
- inability to move the limb with the infected joint
- intense joint pain, swelling, and redness
- fever.
Chills sometimes occur but are an uncommon symptom.
Fibromyalgia
Fibromyalgia may trigger the following symptoms:

- widespread pain, often with specific tender points
- sleep disturbance
- fatigue
- psychological stress
- morning stiffness
- tingling or numbness in hands and feet
- headaches, including migraines
- irritable bowel syndrome
- problems with thinking and memory, sometimes called “fibro fog”
- Painful menstrual periods and other pain syndromes
Psoriatic arthritis
Symptoms of psoriatic arthritis may be mild, affecting only a few joints, such as the finger or toe ends.
Severe psoriatic arthritis, including the spine, can affect several joints. Symptoms of the spinal cord are usually encountered in the lower spine and sacrum. These include stiffness, burning, and pain.
People with psoriatic arthritis also experience psoriasis changes in the skin and hair, and at the same time the skin gets worse as arthritis does.
Gout
Symptoms of gout involve:
- pain and swelling, often in the big toe, knee, or ankle joints
- sudden pain, often during the night, which may be throbbing, crushing, or excruciating
- warm and tender joints that appear red and swollen
- fever sometimes occurs
A person may develop tophi after having gotten gout for several years. Tophi are lumps below the skin , usually around the joints or visible on the fingertips and ears. Multiple, small tophis, or a large white lump, can form. That can cause the skin to bend and stretch.
Often, tophi spontaneously burst out and drain, oozing a thin, chalky substance. Tophi which start breaking through the skin may lead to infection or osteomyelitis. Many patients will require immediate surgery to get the tophus removed.
Sjögren’s syndrome
Symptoms of Sjögren’s syndrome include:
- dry and itchy eyes, and a feeling that something is in the eye
- dry mouth
- difficulty swallowing or eating
- loss of sense of taste
- problems speaking
- thick or stringy saliva
- mouth sores or pain
- hoarseness
- fatigue
- fever
- change in color of hands or feet
- joint pain or joint swelling
- swollen glands
Scleroderma
Symptoms of scleroderma may include:
- fingers or toes that turn blue or white in response to cold temperatures, known as Raynaud’s phenomenon
- hair loss
- skin that becomes darker or lighter than normal
- stiffness and tightness of skin on the fingers, hands, forearm, and face
- small white lumps beneath the skin that sometimes ooze a white substance that looks like toothpaste
- sores or ulcers on the fingertips or toes
- tight and mask-like skin on the face
- numbness and pain in the feet
- pain, stiffness, and swelling of the wrist, fingers, and other joints
- dry cough, shortness of breath, and wheezing
- gastrointestinal problems, such as bloating after meals, constipation, and diarrhea
- difficulty swallowing
- esophageal reflux or heartburn
Systemic lupus erythematosus (SLE)
The most common signs of SLE, or lupus, are:
- red rash or color change on the face, often in the shape of a butterfly across the nose and cheeks
- painful or swollen joints
- unexplained fever
- chest pain when breathing deeply
- swollen glands
- extreme fatigue
- unusual hair loss
- pale or purple fingers or toes from cold or stress
- sensitivity to the sun
- low blood count
- depression, trouble thinking or memory problems.
Many symptoms include mouth sores, unexplained seizures, hallucinations, frequent miscarriages and unexplained problems with the kidney.